Which circumstance supports medical necessity for a payment by the insurance company?
A 64-year-old with congestive heart failure (CHF) has pericardial effusion. The provider inserts a needle under ultrasound guidance, aspirating the fluid from the pericardial sac.
What CPT® coding is reported?
A 58-year-old male suffered an acute STEMI of the inferolateral wall while running a marathon on June 15 and had received treatment. Three weeks later, the patient presents to the ED complaining of SOB and left arm pain. An EKG is performed as well as blood tests. Patient is admitted for further evaluation.
What diagnosis code is reported for this encounter?
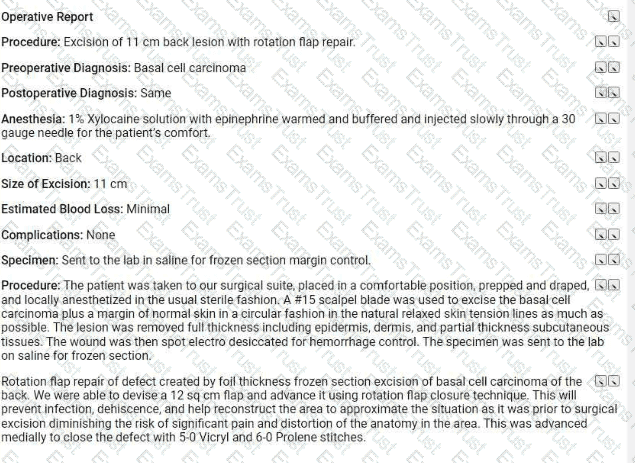
Refer to the supplemental information when answering this question:
View MR 623654
What CPTO coding is reported for this case?
A male patient passes out while jogging in the park. Upon examination at the hospital, he is found to have a wide complex tachycardia and undergoes an electrophysiologic study and radiofrequency ablation. For this procedure he is placed under general anesthesia.
What is the anesthesia coding for this otherwise healthy 35-year-old?
Patient is admitted in observation care on 12/2/20XX in the morning for acute asthma exacerbation. The ED physician requires the patient to stay overnight. Next day, 12/3/20XX the patient is
discharged from observation care in the afternoon. Patient's total stay in observation was 16 hours.
What E/M categories and code ranges are appropriate to report?
A physician sees a patient for the first observation visit, spends 85 minutes, with moderate MDM.
What CPT® code is reported?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What E/M code is reported for this encounter?
A 60-year-old male suffering from degenerative disc disease at the L3-L4 and L5-S1 levels was placed under general anesthesia. Using an anterior approach, the L3-L4 disc space was exposed. Using blunt dissection, the disc space was cleaned. The disc space was then sized and trialed. Excellent placement and insertion of the artificial disc at L3-L4 was noted. The area was inspected and there was no compression of any nerve roots. Same procedure was performed on L5-S1 level. Peritoneum was then allowed to return to normal anatomic position and entire area was copiously irrigated. The wound was closed in a layered fashion. The patient tolerated the discectomy and arthroplasty well and was returned to recovery in good condition. What CPT® coding is reported for this procedure?
A patient who has colon adenocarcinoma undergoes a laparoscopic partial colectomy. The surgeon removes the proximal colon and terminal ileum and reconnects the cut ends of the distal ileum and remaining colon.
What procedure and diagnosis codes are reported?
Which punctuation is used in the ICD-10-CM Tabular List to denote synonyms, alternative wording, or explanatory phrases?
Which entity offers compliance program guidance to form the basis of a voluntary compliance program for a provider practice?
A patient with malignant lymphoma is administered the antineoplastic drug Rituximab 800 mg and then 100 mg of Benadryl.
Which HCPCS Level II codes are reported for both drugs administered intravenously?
A patient is going to have placement of a myringotomy tube. This tube is placed in the ______ to drain excess fluid.
Patient with erectile dysfunction is presenting for same day surgery in removal and replacement of an inflatable penile prosthesis.
What CPT® code is reported for this service?
A healthy 35-year-old undergoes EP study and ablation under general anesthesia.
What anesthesia coding is correct?
Which place of service code is submitted on the claim for a service that is performed in an outpatient surgical floor?
An otolaryngologist performs a tympanoplasty with mastoidectomy, reconstruction of the posterior ear canal wall, and ossicular chain reconstruction.
What CPT® code is reported?
A 52-year-old male patient with known AIDS saw his orthopedic physician today for severe pain in the right knee. The physician documents that his knee pain is due to a flare up of posttraumatic osteoarthritis and he gives him a cortisone injection in the right knee joint. The osteoarthritis is not related to AIDS.
What ICD-10-CM codes are reported for this encounter?
A patient who was training for a marathon collapsed due to heat exhaustion on a very hot day. The patient is driven by his wife to a non-facility urgent care center for him to be treated. On
examination, the physician diagnoses heat exhaustion and dehydration. The physician began IV therapy of normal saline that consists of pre-packaged fluid and electrolytes. The hydration lasts
for 1 and 30 minutes.
What CPT® coding is reported?
A patient suffering from idiopathic dystonia is seen today and receives the following Botulinum injections: three muscle injections in both upper extremities and seven injections in six paraspinal muscles.
How are these injections reported according to the CPT® guidelines?
A patient undergoes angioplasty with stent placement in the left iliac artery.
What CPT® coding is reported?
When a provider’s documentation refers to use, abuse, and dependence of the same substance (e.g., alcohol), which statement is correct?
A patient with abnormal growth had a suppression study that included five glucose tests and five human growth hormone tests.
What CPT@ coding is reported?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What CPT® coding is reported?
An ED provider evaluates a patient with NSTEMI, consults cardiology, and the patient is admitted for PCI.
What E/M service and ICD-10-CM coding is reported by the ED provider?
Dr. Meredith sees Mr. Hollis (new patient) for the first time In the Community Rest Home. She documents a visit with medical decision making of moderate complexity. She spends 20 minutes of additional time discussing physical therapy and going over medications. Dr. Meredith spends a total of 90 minutes on that patient that day.
What CPT® coding does Dr. Meredith report?
Which one of the following is an example of a case in which a diabetes-related problem exists and the code for diabetes is never sequenced first?
When a patient has ESRD, which system is affected?
A 20-year-old female is being seen for the first time by a primary care physician to have a yearly physical. During the examination for the physical, the provider discovers non-inflammed lesions on her legs and arms. The physician performs a complete physical and additional separate documentation for the treatment of the lesions on the bilateral upper and lower extremities. The provider has the patient buy an over-the-counter ointment and will continue to watch them.
What CPT® coding is reported for this visit?
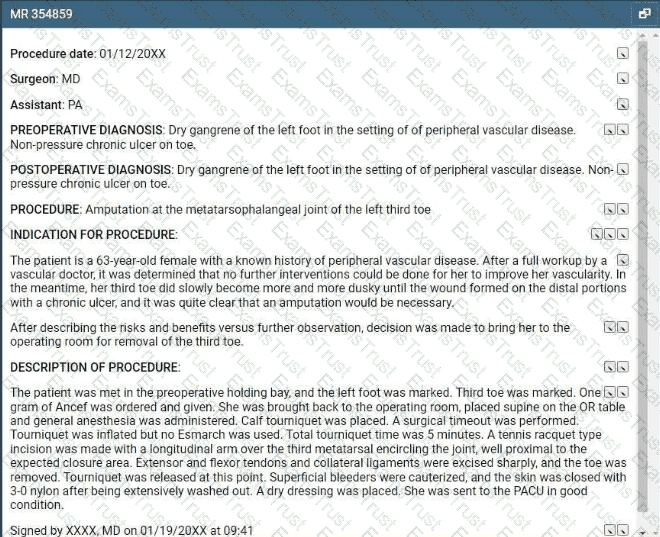
Refer to the supplemental information when answering this question:
View MR 354859
What CPT® and ICD-10-CM coding is reported?
A patient with Parkinson's has sialorrhea. The physician administers an injection of atropine bilaterally into a total of four submandibular salivary glands.
What CPT® coding is reported?
Which medical term refers to inflammation of the cornea?
A patient with end-stage renal disease (ESRD) receives hemodialysis 3x weekly in the office for one month. The nephrologist performs a comprehensive exam and supervises dialysis.
What CPT® and ICD-10-CM codes are reported?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What CPT® and ICD-10-CM codes are reported?
An interventional radiologist performs an abdominal paracentesis in his office utilizing ultrasonic imaging guidance to remove excess fluid. What CPT® coding is reported?
Miranda is in her provider's office for follow up of her diabetes. Her blood sugars remain at goal with continuing her prescribed medications.
When referring to the MDM Table in the CPT® code book for number and complexity of problems addressed at the encounter, what type of problem is this considered?
A provider performs a mastoidectomy and complete labyrinthectomy for right-sided peripheral vertigo.
What CPT® and ICD-10-CM codes are reported?
A 5-year-old who has an allergy history experienced a possible reaction to peanuts. A quantitative, high-sensitive fluorescent enzyme immunoassay was used to measure specific IgE for recombinant peanut components. Results showed there was no reaction indicating the child has a peanut allergy.
What lab test is reported?
Which punctuation is used in the ICD-10-CM Alphabetic Index to identify manifestation codes?
A 50-year-old patient presented with a persistent cough has not responded to standard treatments. The patient's physician decides to perform a flexible bronchoscopy with bronchial biopsies to further investigate the cause. A flexible bronchoscope is inserted through the patient's mouth and into the bronchial tubes. Five biopsies are taken for further testing. The biopsies were sent to the lab for analysis to determine the next steps in the patient's treatment plan.
What CPT® coding is reported?
A wedge excision of soft tissue at the lateral margin of an ingrown toenail on the left great toe is performed.
What CPT® code is reported?
A 55-year-old female patient is diagnosed with renal cell carcinoma. She is having a resection of the affected kidney, a portion of the ureter, and rib resection, open aproach. The procedure is complicated due to a prior surgical procedure performed on the same kidney.
What CPT® coding is reported?
A physician excises a 3.5 cm malignant lesion including margins from the back. Then a destruction of a 2.0 cm benign lesion on the right cheek of the face with cryosurgery.
What CPT@ and ICD-10-CM is reported?
View MR 002395
MR 002395
Operative Report
Pre-operative Diagnosis: Acute rotator cuff tear
Post-operative Diagnosis: Acute rotator cuff tear, synovitis
Procedures:
1) Rotator cuff repair
2) Biceps Tenodesis
3) Claviculectomy
4) Coracoacromial ligament release
Indication: Rotator cuff injury of a 32-year-old male, sustained while playing soccer.
Findings: Complete tear of the right rotator cuff, synovitis, impingement.
Procedure: The patient was prepared for surgery and placed in left lateral decubitus position. Standard posterior arthroscopy portals were made followed by an anterior-superior portal. Diagnostic arthroscopy was performed. Significant synovitis was carefully debrided. There was a full-thickness upper 3rd subscapularis tear, which was repaired. The lesser tuberosity was debrided back to bleeding healthy bone and a Mitek 4.5 mm helix anchor was placed in the lesser tuberosity. Sutures were passed through the subcapulans in a combination of horizontal mattress and simple interrupted fashion and then tied. There was a partial-thickness tearing of the long head of the biceps. The biceps were released and then anchored in the intertubercular groove with a screw. There was a large anterior acromial spur with subacromial impingement. A CA ligament was released and acromioplasty was performed. Attention was then directed to the
supraspinatus tendon tear. The tear was V-shaped and measured approximately 2.5 cm from anterior to posterior. Two Smith & Nephew PEEK anchors were used for the medial row utilizing Healicoil anchors. Side-to-side stitches were placed. One set of suture tape from each of the medial anchors was then placed through a laterally placed Mitek helix PEEK knotless anchor which was fully inserted after tensioning the tapes. A solid repair was obtained. Next there were severe degenerative changes at the AC joint of approximately 8 to 10 mm. The distal clavicle was resected taking care to preserve the superior AC joint capsule. The shoulder was thoroughly lavaged. The instruments were removed and the incisions were closed in routine fashion. Sterile dressing was applied. The patient was transferred to recovery in stable condition.
What CPT® coding is reported for this case?
A patient is having X-ray imaging of his abdomen following a traumatic episode. A decubitus, supine, and erect views are performed on the abdomen.
What CPT® is reported?
Provider performs staged procedures for gender reassignment surgery converting female anatomy to male anatomy.
What CPT® code is reported?
When a provider's documentation refers to use, abuse, and dependence of the same substance (e.g. alcohol), which statement is correct?
A 42-year-old male is diagnosed with a left renal mass. Patient is placed under general anesthesia and in prone position. A periumbilical incision is made and a trocar inserted. A laparoscope is inserted and advanced to the operative site. The left kidney is removed, along with part of the left ureter. What CPT® code is reported for this procedure?
A suppression study includes five glucose tests and five growth hormone tests.
What CPT® coding is reported?
A surgeon performs a complete bilateral mastectomy with insertion of breast prosthesis at the same surgical session.
What CPT@ coding is reported?
A patient who was experiencing severe abdominal pain underwent abdominal imaging and results showed several peritoneal tumors of various sizes.
The patient elected to have the tumors removed. An incision was made to access the intra-abdominal peritoneal cavity, where four tumors were identified, measured, and excised.
The largest was 2 cm, two were 1 cm each, and the smallest was 0.5 cm. Pathology report indicated the tumors were malignant.
What CPT® and ICD-10-CM coding is reported7
View MR 007400
MR 007400
Radiology Report
Patient: J. Lowe Date of Service: 06/10/XX
Age: 45
MR#: 4589799
Account #: 3216770
Location: ABC Imaging Center
Study: Mammogram bilateral screening, all views, producing direct digital image
Reason: Screen
Bilateral digital mammography with computer-aided detection (CAD)
No previous mammograms are available for comparison.
Clinical history: The patient has a positive family history (mother and sister) of breast cancer.
Mammogram was read with the assistance of GE iCAD (computerized diagnostic) system.
Findings: No dominant speculated mass or suspicious area of clustered pleomorphic microcalcifications is apparent Skin and nipples are seen to be normal. The axilla are unremarkable.
What CPT® coding is reported for this case?
Mr. Roland has difficulty breathing and congestion with a productive cough. The physician takes frontal and lateral view chest X-rays in the office (the equipment is owned by the physician group). The physician reads the X-rays and determines a diagnosis of walking pneumonia. The physician’s interpretation is placed in the patient’s chart.
How does the physician bill for the chest X-ray?
A patient has chronic cholesteatoma in the right middle ear. The otolaryngologist performed a tympanoplasty with a radical mastoidectomy, removing the middle ear cholesteatoma. Grafting technique was used to repair the eardrum without ossicular chain reconstruction.
What CPT® code is reported for this surgery?
911 is called by the physician for an ambulance with non-emergency basic life support to pick up a patient from his office that had fainted. The patient was taken to the hospital. What HCPCS
Level II coding is reported for the ambulance's service?
The procedure is performed at an outpatient radiology department. From a left femoral access, the catheter is placed in the abdominal aorta and is then selectively placed in the celiac trunk and manipulated up into the common hepatic artery for an abdominal angiography. Dye is injected, and imaging is obtained. The provider performs the supervision and interpretation.
What CPT® codes are reported?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What CPT® and ICD-10-CM codes are reported?
A patient has five biopsies performed on the duodenum.
What CPT® coding is reported?
A patient presents with 26 skin tags on the neck and shoulder. The provider removes all using a scissoring technique.
What CPT® coding is reported?
A 74-year-old arrived at the ED experiencing bright red rectal bleeding when using the toilet. She does not have any abdominal pain, no nausea or vomiting. She has been undergoing dialysis for
years due to end-stage renal failure and has a diagnosis of myelodysplastic syndrome with a platelet count of just 3,000. Her hemoglobin level, which was 10 at her dialysis session the
previous day, dropped to 7. Abdominal films are negative. An urgent esophagogastroduodenoscopy (EGD) was performed, and no active bleeding was found in the esophagus or the stomach.
However, the scope was passed into the upper duodenum which did reveal some oozing, and was controlled with cautery. Next, the patient was then positioned on her left side for a
colonoscopy that extended from the colon to the ileum and into the lower duodenum, but no definitive sources of bleeding were found. Again, no outright bleeding sources were identified. A
CRNA performed the anesthesia and documented PS III.
What CPT® codes are reported for the CRNA?
A 5-year-old patient has a fractured radius. The orthopedist provides moderate sedation and the reduction. The time is documented as 21 minutes.
What CPT® code is reported for the moderate sedation?
A patient presents to the ER from a nursing home after the patient was found to have foul smelling, large sacral pressure ulcer during daily nursing rounds. The ER provider swabbed the wound
for culture (which measured at 7cm in largest diameter); then cleaned the site before painting with povidone around the entire sacrum to reduce cutaneous bacterial load. The provider made an
elliptical excision with 3mm margins around the outer edge of the ulcer and removed the lesion in its entirety. Further examination revealed deep tissue damage, prompting muscle and
segmental bone removal. The wound was then closed using a layered skin flap closure.
What CPT® coding and ICD-10-CM coding is reported?
A woman at 36-weeks gestation goes into labor with twins. Fetus 1 is an oblique position, and the decision is made to perform a cesarean section to deliver the twins. The obstetrician who delivered the twins, provided the antepartum care, and will provide the postpartum care.
What CPT® coding is reported for the twin delivery?
Patient is diagnosed with dacryocystitis, which is the inflammation of?
A patient arrives for a PEG placement. The patient requires tube feeds for nutrition but frequently pulls out the dobhoffs tube. An EGD was performed. Several attempts were made to place the
PEG tube without success so the procedure was aborted. During the withdraw of the scope, a small hiatal hernia was noted in the stomach. The scope was removed the the patient transferred
to recovery.
What CPT and ICD-10-CM coding is reported?
Refer to the supplemental information when answering this question:
View MR 903096
What CPT® and ICD-10-CM coding is reported?
Repeat three-view imaging of both hips and pelvis is performed on the same day due to a new fall, interpreted by the same radiologist.
What CPT® coding is reported?
A planned partial meniscectomy of the temporomandibular joint is cancelled after anesthesia and incision due to respiratory distress.
What CPT® coding is reported for the oral surgeon?
The gynecologist performs a colposcopy of the cervix including biopsy and endocervical curettage.
What CPT® code is reported?
A patient with jaundice was seen by the physician to obtain liver biopsies. A needle biopsy was taken using CT guidance for needle placement. The physician obtained two core biopsies, which
were then sent to pathology. What CPT® codes are reported?
A surgeon performed Mohs micrographic surgery on a lesion on the right arm. This required one stage with six tissue blocks.
What CPT@ codes are reported for the Mohs surgery?
An interventional radiologist performs an abdominal paracentesis using fluoroscopic guidance to remove excess fluid. The procedure is performed in the hospital. What CPT® coding is reported?
A 47-year-old male recently injured as a passenger in a car accident sustained multiple fractures. The patient now has physical restraints due to pulling out foley catheter, IV catheters and
attempted to pull out NG tube. Emergency department physician is asked to come see patient and injects 0.5 lidocaine into lumbar region of the spine. An indwelling catheter is placed into the
lumbar region for continuous infusion with fluoroscopy for pain management.
What CPT® is reported for the Emergency department physician?
An established patient presents with fever and sore throat. Rapid strep test is positive.
What CPT® and ICD-10-CM codes are reported?
A patient with suspected gynecologic malignancy undergoes laparoscopic staging including bilateral pelvic lymphadenectomy, periaortic lymph node sampling, peritoneal washings, peritoneal and diaphragmatic biopsies, and omentectomy.
What CPT® coding is reported?
A patient presents for planned sterilization via bilateral excisional vasectomy.
What CPT® and ICD-10-CM codes are reported?
A 35-year-old female has cancer in her left breast. The surgeon performs a mastectomy, removing the breast tissue, skin, pectoral muscles, and surrounding tissue, including the axillary and internal mammary lymph nodes.
Which mastectomy code is reported?
A patient is brought to the operating room with a right-sided peripheral vertigo. The provider makes a postauricular incision and uses an operating microscope to perform a mastoidectomy using a burr. He next destroys the semicircular canals, the utricle, and saccule completely removing the diseased labyrinth structures. The provider sutures the incision.
What CPT® code and ICD-10-CM codes are reported?
A patient in a radiology facility has an X-ray examination of her thoracolumbar junction due to pain while playing golf. The patient also has limited mobility in the hip. A radiologist takes a two view of the thoracolumbar junction.
What CPT® code is reported'
A 1-year-old is with his mom to have his scheduled vaccinations. The physician provides counseling for routine immunizations and carries out measles, mumps, rubella and varicella (MMRV)
subcutaneously and dose 3 of Hepatitis B intramuscularly without difficulty.
What CPT® codes are reported?
A 46-year-old female is admitted to the hospital by her urologist for a left ureteral calculus. The urologist visits her again on day two and performs a low for number and complexity of problems
addressed, minimal for amount and/or complexity of data to be reviewed and analyzed, and moderate for risk of complications.
What E/M service is reported for day two?
A pediatric patient with a congenital double inlet ventricle undergoes corrective cardiac surgery. The surgeon performs a modified Fontan procedure to redirect systemic venous blood flow directly to the pulmonary arteries as part of staged repair for a single-ventricle physiology.
What CPT® and ICD-10-CM® codes are reported?
A patient who has colon adenocarcinoma undergoes an open partial colectomy. The surgeon removes the proximal colon and terminal ileum and reconnects the cut ends of the distal ileum and
remaining colon.
What procedure and diagnosis codes are reported?
The surgeon performs Roux-en-Y anastomosis of the extrahepatic biliary duct to the gastrointestinal tract on a 45-year-old patient.
What CPT® code is reported?
A provider orders LC-MS definitive drug testing for suspected acetaminophen overdose.
What CPT® code is reported?
Which statement is FALSE in reporting a personal history ICD-10-CM code?
Dr. Carter sees Mrs. White at the Spring Valley Nursing Facility. He saw her last month after she was admitted to the facility. Today is a follow up visit. She is doing well. He documented a medically appropriate history and exam. The patient has osteoporosis, hypertension, dementia. CAD, CHF, and type 2 diabetes (moderate number and complexity of problems). He reviews 4 labs and a telemetry (Moderate data). He adds a Cardizem prescription for better control of her blood pressure which is a moderate risk. What CPT® code does Dr. Carter report for the visit?
A patient was in a car accident as the driver and suffered a concussion with brief loss of consciousness (15 minutes). What ICD-10-CM codes are reported?
A patient with empyema requires a Schede thoracoplasty.
What CPT® code is reported for this procedure?
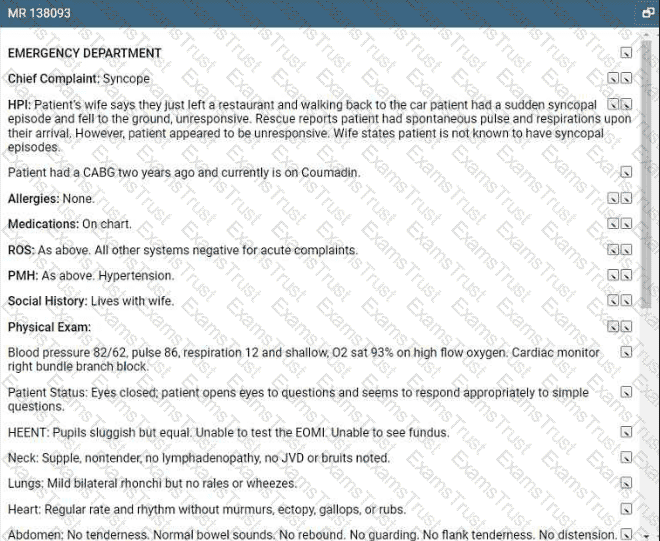
Refer to the supplemental information when answering this question:
View MR 138093
What E/M coding is reported?
A child returns for stage 2 surgical repair of double outlet right ventricle, including removal of pulmonary artery band, arterial switch repair, and ECMO cannulation.
What CPT® codes are reported?
A patient is diagnosed with a pressure ulcer on her right heel that is currently being treated.
What ICD-10-CM code is reported?
A patient has nausea with several episodes of emesis along with severe stomach pain due to dehydration. Normal saline is infused in the same bag with 2 mg ondansetron to help with the
nausea. Then a dose of 15 mg ketorolac tromethamine was given for the stomach pain.
What J codes are reported for these services?
A patient receives 200 mg IM Depo-Testosterone.
What HCPCS Level II coding is reported?
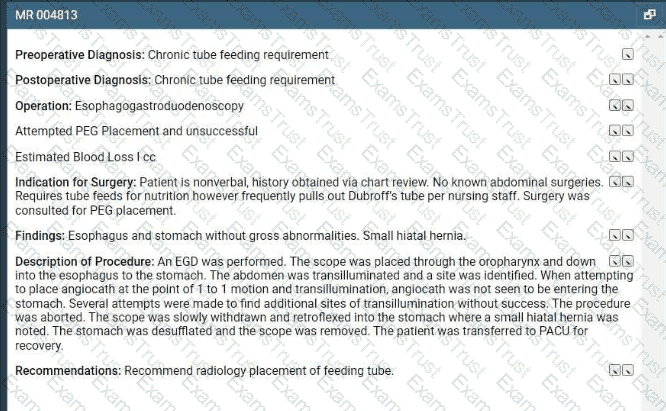
Refer to the supplemental information when answering this question:
View MR 004813
What CPT® and ICD-10-CM codes are reported?
A 65-year-old man had a right axillary block by the anesthesiologist. When the arm was totally numb, the arm was prepped and draped, and the surgeon performed tendon repairs of the right first, second, and third fingers. The anesthesiologist monitored the patient throughout the case.
What anesthesia code is reported?
A patient with multiple atypical lesions on the face and trunk is in the office to perform a biopsy. A punch tool was used to obtain a full-thickness tissue sample for two lesions on the trunk.
Partial-thickness tissue sample was taken from one lesion on the forehead using a curette.
What CPT® coding is reported?
Preoperative diagnosis: Right thigh benign congenital hairy nevus. *1
Postoperative diagnosis: Right thigh benign congenital hairy 0 nevus.
Operation performed: Excision of right thigh benign congenital>1
nevus, excision size with margins 4.5 cm and closure size 5 cm.
Anesthesia: General.0
Intraoperative antibiotics: Ancef.0
Indications: The patient is a 5-year-old girl who presented with her parents for evaluation of her right thigh congenital nevus. It has been followed by pediatrics and thought to have changed over the past year. Family requested excision. They understood the risks involved, which included but were not limited to risks of general
anesthesia, infection, bleeding, wound dehiscence, and poor scar formation. They understood the scar would likely widen as the child grows because of the location of it and because of the age of the patient. They consented to proceed.
Description of procedure: The patient was seen preoperatively in > I the holding area, identified, and then brought to the operating room. Once adequate general anesthesia had been induced, the patient's right thigh was prepped and draped in standard surgical fashion. An elliptical excision measuring 6 x 1.8 cm had been marked. This was injected with Lidocaine with epinephrine, total of 6 cc of 1% with 1:100,000. After an adequate amount of time, a #15 blade was used to sharply excise this full thickness.
This was passed to pathology for review. The wound required □ limited undermining in the deep subcutaneous plane on both sides for approximately 1.5 cm in order to allow mobilization of the skin for closure. The skin was then closed in a layered fashion using 3-0 Vicryl on the dermis and then 4-0 Monocryl running subcuticular in the skin, the wound was cleaned and dressed with Dermabond and Steri-Strips.
The patient was then cleaned and turned over to anesthesia for S extubation.
She was extubated successfully in the operating room and taken S to the recovery room in stable condition. There were no complications.
What is the radiology coding for this encounter?
A patient has suspicious lesions on his feet. Biopsies confirm squamous cell carcinoma. The patient elects to destroy a 0.6 cm lesion on the right dorsal foot and a 2.0 cm lesion on the left dorsal foot using cryosurgery.
What CPT® coding is reported?
An 8-year-old undergoes tonsillectomy with adenoidectomy for chronic tonsillitis and adenoiditis with hypertrophy.
What CPT® and ICD-10-CM codes are reported?
A patient presents with recurrent spontaneous episodes of dizziness of unclear etiology. Caloric vestibular testing is performed irrigating both ears with warm and cold water while evaluating the patient’s eye movements. There is a total of three irrigations.
What CPT® coding is reported?
An autopsy is ordered for a deceased patient of unknown cause. The pathologist performs gross and microscopic examination, including the brain and spinal cord.
What CPT® coding is reported?
A physician conducts a 15-minute phone call discussing medication management.
How is this reported?
What is the HCPCS Level II code for a standard wheelchair?
An anesthesiologist medically directs two cases during EGD and colonoscopy in a PS III patient with severe bleeding risk.
What CPT® codes are reported?